Pancreatic Surgery
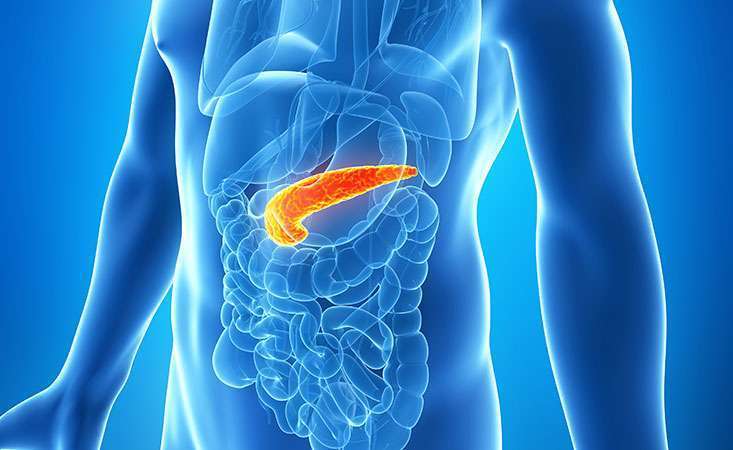
Introduction to the Pancreas
The pancreas is a vital organ located just below the liver and in the retroperitoneal space (anatomical space at the back of the abdomen). It has both exocrine (digestive enzymes) and endocrine (hormones) functions and plays a key role in maintaining blood glucose levels. The exocrine function of the pancreas involves the secretion of enzymes into the duodenum to aid in the digestion and absorption of nutrients. The endocrine function involves secretions of hormones to regulate blood glucose levels.
What is Pancreas Disease?
The pancreas can be affected by a variety of diseases and injuries. Pancreas diseases can be classified as either acute or chronic. The most common acute disease of the pancreas is acute pancreatitis (inflammation of the pancreas).
Some of the causes of acute pancreatitis are:
- Helps in the digestion of fat via the production of bile
- Conversion of carbohydrate (sugar) into energy
- Produces blood clotting factors
- Aids in excretion of waste product
- Protects against infection
- Regulates cholesterol level
- Metabolism and elimination of drugs and toxins
Gallstones and alcohol are the two most common causes of acute pancreatitis in the Western world. Recurrent acute pancreatitis can lead to chronic pancreatitis. The most common cause of chronic pancreatitis is excessive alcohol consumption.
Other potential causes for chronic pancreatitis are:
- Congenital anatomical variant of the pancreatic duct
- Genetic factors
- Cystic fibrosis
Symptoms of Pancreatic Disease
There are no specific symptoms that can be attributed to pancreatic disease, which contributes to the late diagnosis of pancreatic cancer with vague symptomology.
Symptoms can include:
- Upper abdominal (epigastric) discomfort/pain that radiates to the back
- Back pain
- Nausea and lack of appetite
- Jaundice if the bile duct was obstructed by an abnormality at the head of the pancreas. Patients would report dark urine, pale stools, itchy skin, and yellow-tinged eyes.
- Steatorrhoea due to a lack of secretion of digestive (exocrine) enzymes by the pancreas. This is characterised by loose, pale, floating, and offensive-smelling bowel motions secondary to fat malabsorption in the intestine.
- New-onset diabetes if the endocrine function of the pancreas is impaired by the cancer.
What is Pancreatic Surgery?
Pancreatic surgery refers to a variety of surgical procedures that can be performed on the pancreas. Pancreatic surgery usually includes removing part of the pancreas, most commonly for pancreatic cancer. Occasionally, it can be performed for pre-cancerous lesions.
The more common pancreatic surgery include:
- Pancreaticoduodenectomy (Whipple’s procedure)
- Distal pancreatectomy
- Total pancreatectomy
The type of surgery depends on the indication for surgery. During your consultation, Dr. Michael Chu will discuss the indications and what the surgery involves.
Pre-Operative Assessment
Initial Assessment
Initial assessment will include blood tests (including CA19-9) and imaging of your pancreas (USS, CT, and/or MRI) to assess the extent of the pancreas cancer. These are performed to determine your suitability for pancreatic surgery. The results of these investigations will be discussed with you, and treatment options will be outlined.
Anaesthetic Assessment
Once a decision has been made to proceed with surgery, you will be requested to fill out an anaesthetic questionnaire. This will be reviewed by the anaesthetist responsible for your care and you may be required to see the anaesthetist in person or sent for additional tests. Once you have completed the anaesthetic review, the date of surgery will be confirmed with you.
Types of Pancreatic Resection
The two most common types of pancreatic resection are the Whipple’s procedure and distal pancreatectomy. The type of resection is dependent on the site of the cancer. Whipple procedures are an open procedure (laparotomy) while in certain cases, it is feasible to perform distal pancreatectomy laparoscopically (keyhole). In rare occasions, a total pancreatectomy (complete removal of the pancreas) is indicated (if there is a large tumour or more than one tumour).
Pancreaticuduodenectomy (Whipple’s Procedure)
This is performed for lesions at the head of the pancreas. An incision is made in the right upper quadrant of the abdomen and the abdominal cavity is entered into carefully. The incision can be a straight midline wound or, more commonly, a “Reverse-L incision”.
The head of the pancreas will be removed with the following organs and tissues:
- Distal (lower) end of the stomach
- Duodenum
- Gallbladder
- Lower part of the bile duct
- Lymph nodes (lymphadenectomy)
These are removed concurrently to completely remove the cancer and because they share the same blood supply as the head of the pancreas. Once the resection phase has been completed, the pancreas, bile duct, and stomach are reconnected to the jejunum (small bowel).
The procedure will be explained with the aid of a diagram during your consultation with Dr. Michael Chu.
Distal Pancreatectomy +/- Splenectomy
This is performed for lesions at the tail and body of the pancreas. If the indication is pancreas cancer, the spleen will also be removed. In pre-malignant cases, the spleen can be preserved. The reason for the removal of the spleen is to obtain adequate clearance for the cancer and the surrounding lymph nodes, necessitating the removal of the splenic vessels, which sit on top of the pancreas.
Distal pancreatectomy can be performed via a laparotomy or laparoscopic technique, depending on the pancreas cancer. A laparotomy is usually performed via a midline wound. For laparoscopic distal pancreatectomy, a laparoscope (camera) is introduced via a small incision and three further small wounds are used to allow the utility of laparoscopic surgical instruments. Once the pancreatic resection has been completed, the wound for the laparoscope is extended to allow removal of the resected pancreas +/- spleen.
Risk of Surgery
Any surgery has risks, which can be divided into “General” or “Procedure-specific risks.” Pancreatic surgery is complex, and recovery can be long.
General Risks
- Wound infection
- Venous thromboembolism (VTE), e.g., deep vein thrombosis (DVT) or pulmonary embolism (PE)
- Incisional hernia at the wound site
- Respiratory complications such as pneumonia (infection) or atelectasis (collapse) can occur secondary to poor inspiratory effort in the post-operative period and from prolonged ventilator support. This can usually be treated with antibiotics and may occasionally require drainage. To reduce the risk of post-operative respiratory complications, it is important for early mobilisation in the post-operative period to help expand the lungs.
Procedure-Specific Risks from Pancreas Resection
There are some rare but specific complications related to pancreatic resection:
- Pancreatic leak
This is when pancreatic fluid leaks out from the anastomosis (joining of small bowel to the pancreas) in Whipple’s procedure or from the cut surface of the pancreas in distal pancreatectomy. There will be a drain left in the abdominal cavity in all pancreatic resections and the fluid collected will be tested for amylase (one of the pancreatic enzymes). This will allow us to detect for a pancreatic leak. In the majority of cases, the leak is mild and will self-resolve. Occasionally, further procedures may be required.
- Bile leak
This occurs when the anastomosis of the bile duct to the small intestine leaks bile fluid into the abdomen. This is a rare occurrence and will generally self-resolve.
- Post-operative bleeding
This usually occurs in the setting of a pancreatic leak and may require radiological intervention to stop the bleeding from within the blood vessel (angiogram & embolisation). Rarely, a re-operation may be required.
- Post-operative infection in setting of Splenectomy
The spleen aids the body in fighting infection, particularly against encapsulated organisms. If the spleen is removed, you will be more prone to infections caused by these organisms. In that case, you will be given vaccination against these organisms to reduce the risk against these organisms.
Contraindications to Pancreatic Surgery
All patients undergo a thorough assessment before deciding whether to proceed with pancreatic surgery. This will include clinical examination, blood tests, and advanced imaging (CT or MRI Pancreas). Dr. Michael Chu will work alongside you at each step of the assessment and make sure you have a thorough understanding. If the potential benefit from surgery is less than the risks of surgery, surgery would not be recommended.
Post-Operative Management
Depending upon the extent of the pancreatic resection, you may be required to be admitted to the High Dependency Unit (HDU) for the night of your surgery. You will be cared for on the ward after your HDU stay. There will be several checks performed by the nursing staff routinely, including overnight.
During your hospital stay, Dr. Michael Chu will review you twice a day, and the anaesthetist will review you at least once a day. The ward staff are very experienced in caring for patients following pancreatic surgery and will be caring for you.

Post-operative Diet
Patients are allowed to eat and drink as tolerated following surgery. On the night following surgery in HDU, patients are allowed to drink oral fluids as tolerated and then progress to a full diet as tolerated in the next 24-48 hours. Please ensure that you listen to your body with regard to appetite/hunger. If you feel full/bloated, do not try to push more oral intake. If required, a dietitian will visit you on the ward to advise you about post-operative dietary requirements and prescribe supplemental nutrition drinks as needed.
In the initial stages, you may find that eating small meals regularly throughout the day may be more tolerable than three large meals a day. As you improve, you will be able to adjust your dietary intake to suit your body. If you are really struggling with your oral intake, dietary supplements are available, which can be liaised with a dietitian.
Post-Operative Mobility
You will be encouraged to mobilise as much as possible during your hospital stay to reduce the risk of post-operative lung complications and DVT. In the first post-operative day (this may be in HDU), you will be encouraged and assisted to mobilise into a chair, sometimes for a short distance.
Post-Operative Analgesia
The majority of patients will have mild discomfort post-operatively. Pain management will be managed between Dr. Michael Chu and the anaesthetist. It usually consists of regular paracetamol with the addition of stronger analgesia (in the form of opioids) on an “as required” (PRN) basis.
Prophylaxis for Blood Clots (VTE)
To prevent VTE, patients will require a daily injection to be self-administered subcutaneously in the abdomen. This will be for 28 days post-operatively and patients will be instructed on how to administer this prior to their discharge.
Wound Care
The surgical incision will be sutured with dissolvable sutures and do not require removal. Steristrips (thin-adhesive bandages) are placed over the incision to support the skin edge and reduce the tension on the wound; they are usually on for 10 days. On top of the Steristrips, a waterproof dressing is placed and should stay for at least 3-5 days. You can shower with this dressing, and it should be pat dry afterwards. Some patients prefer to leave the waterproof dressing for a bit longer, and that is okay. If the Steristrips fall off earlier than 10 days, it is acceptable.
Once the dressing is removed and the wound appears clean and dry, the wound does not need further dressings. Occasionally, the wound may leak some “dark-ish” fluid or look a little red, and this is not unusual. The staff will keep a close eye on the wound. If staples or non-dissolvable sutures are used to close the wound, these will need to be removed after 10-14 days. The district nurse will be able to do this for you. If you would like to use Vitamin E or Bio-Oil on the wound to reduce scar prominence, please do so after the first week.
Duration of Hospital Stay
The majority of patients spend 5-6 days in hospital prior to discharge. The general criteria for discharge are:
- Mobilising independently
- Have an adequate oral intake (fluids and food),
- Able to perform the majority of self-care
- Only requiring oral analgesia.
Post-Operative Activity
- Activity & Work
Patients are allowed to perform their regular activities as long as it is not too uncomfortable for them. However, it is recommended to avoid heavy lifting or activity for 4-6 weeks. Most patients do return back to work after this period but some may take longer to do so. It normally takes ~3 months to return to normal activities. Additionally, most patients experience reduced energy levels post-operatively for a few weeks (can be up to 6-8 weeks). Please be patient and give yourself time to recover.
- Driving
It is recommended that patients not drive for a minimum of 3 weeks post-pancreatic surgery. When you get home and feel ready to drive, sit in the car seat and ensure you are able to perform a full emergency stop/brake before you start driving. It is also advisable that you have the strength to control the car and respond quickly before you start driving.
Importantly, please check with your insurance policy and company to ensure that driving post-operatively does not invalidate your policy.
Tubes & Drains
- Feeding Tube
The feeding tube passes through the nose into the stomach and allows supplementary nutrition to be administered in the post-operative period in conjunction with a dietitian.
- Drain
A drain will be routinely inserted during pancreatic surgery. It allows drainage of any fluid (blood, pancreatic fluid, or bile) that may leak out. The drain will be left in place for at least three days.
- Urinary Catheter
A catheter is placed in the urinary bladder in the operating theatre to monitor urine output (kidney function) during the post-operative period. This is usually removed on post-operative day 2.
Post-Discharge Management
When should I seek medical input?
If you or your family have any concerns, please contact Dr. Michael Chu directly, his rooms, or the hospital. If it is a medical emergency, please dial 111 for an ambulance to take you to the nearest acute hospital.
How does my General Practitioner (GP) know about my surgery?
Dr. Michael Chu will send a letter to your GP summarising your hospital stay and a copy of your operation note to keep your GP up-to-date with your status. It is advisable that you make an appointment with your GP a few days after your discharge so they can physically assess your clinical status.
Dr. Michael Chu is happy to be contacted by your GP if they have any questions or concerns.
Common side-effects of surgery & solutions
- Pain or discomfort
After an operation, a degree of discomfort is expected and usually improves over the first two weeks. In some patients, the discomfort may last for a few weeks. The aim of the prescribed analgesia is to ensure that the discomfort is manageable so that you can continue to improve physically. However, if the pain is worsening or you have any concerns about its duration (greater than two weeks), please contact your GP or Dr. Michael Chu
- Bruising
There is usually bruising around the incision, which may extend up to the ribs. The bruising may appear within 24-48 hours after surgery. If you feel that the bruising is worsening, becoming painful, or there is discharge of pus from the wound, please contact Dr. Michael Chu.
- Constipation
This is a common occurrence following any abdominal surgery. It is usually related to the opioids during general anaesthetic or those given post-operatively for analgesia. A few laxatives can be obtained over the counter at the pharmacy or by prescription. Similarly, natural dietary supplements such as kiwi fruit are also quite effective. Importantly, please drink plenty of fluid.
Frequently Asked Questions about Liver Surgery
What is the recovery period?
The recovery period is at least 6-8 weeks before returning to normal activity. However, your gut function may take up to 6 months to normalise. You are encouraged to eat small regular meals rather than three large meals a day.
Do I need further chemotherapy after pancreatic surgery?
This is dependent on the final pathology results and your clinical status following surgery. Each case is unique and will be discussed with an oncologist (medical cancer specialist), who is the specialist providing the chemotherapy.
What do I need to do to prepare for surgery?
Once a proposed date for surgery has been set, you will need to follow these instructions:
- Blood tests are taken 1-2 days prior to the day of surgery. This ensures that blood is available if you require a blood transfusion.
- Specific instructions will be given on where and when to present for surgery.
- Specific instructions will be given on when to stop drinking and eating. It is important that you follow these instructions as it will pose an anaesthetic risk, and we may have to cancel or delay your surgery.
- You do not need to shave before coming into the hospital.
- You will be advised on what normal medications to take on the day of surgery, but only take them with a small amount of water.
- If you are on any blood thinners that affect clotting, please inform Dr. Michael Chu during your consultation, as they may need to be stopped well in advance before the day of surgery. If you are unsure about any medications, please ask Dr. Michael Chu and the anaesthetist.
What is the follow-up process for me?
A follow-up will be arranged for you after you have been discharged from the hospital. Dr. Michael Chu's PA will get in contact with you, and the follow-up is usually 1-2 weeks after leaving the hospital.
At the follow-up consultation, Dr Michael Chu will go through with you:
- How you are recovering
- Operative findings
- Pathology report from the surgery
Depending on your recovery and the pathology result, Dr. Michael Chu may recommend additional investigations, treatment, or follow-up reviews. Dr Michael Chu will ensure you are fully aware of the plan and answer any questions that may arise during the consultation.
If you have any questions or concerns during your post-operative period, please contact Dr. Michael Chu at +64 27 216 7288.
