Cholecystectomy
What is a Laparoscopic Cholecystectomy?
Cholecystectomy is the removal of the gallbladder, and laparoscopic is the term for keyhole surgery where a laparoscope (tube-like camera) is used inside the abdominal cavity. Cholecystectomy can also be performed via an open (laparotomy) approach and is usually reserved for gallbladder cancer.

Indications for Cholecystectomy
The most common indication for cholecystectomy is the presence of gallstones and symptoms related to gallstones.
The other common indication for a cholecystectomy is the presence of gallbladder polyps. Gallbladder polyps are small growths that arise from the gallbladder lining, and they are diagnosed with an ultrasound scan. The reason for the removal of gallbladder polyps is the risk of developing gallbladder cancer over a long period.
The risk of developing gallbladder cancer is related to the size of the polyp, and treatment/surveillance options are based on the size of the polyp.
- Less than 7 mm in size: Not associated with the development of cancer. Ultrasound surveillance at 1-2 yearly intervals would be recommended.
- 7-9 mm in size: Rare association with the development of cancer. Regular 6-monthly ultrasound surveillance may be recommended.
- Greater than 10 mm in size: 10% of patients will develop gallbladder cancer. A cholecystectomy is recommended in suitable patients.
How is a Laparoscopic Cholecystectomy performed?
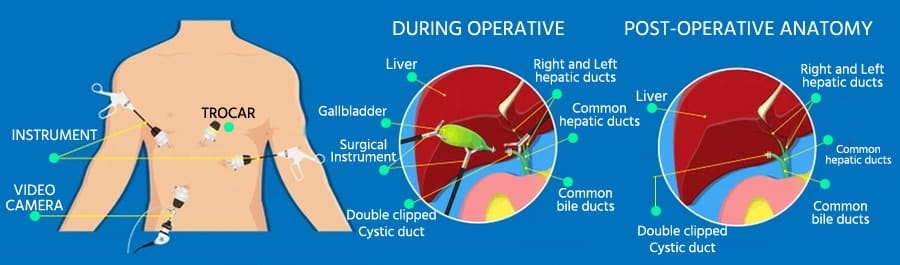
There are usually four small incisions made on the abdomen, with one around the umbilicus. The position of these incisions may vary between patients. Once access into the abdomen has been established, a laparoscope (telescope) is placed through one of the small incisions to allow visualisation of the inside of the abdominal cavity. Ports (hollow tubes) are then inserted through the other incisions. Carbon dioxide is used to insufflate the abdomen to lift the abdominal wall away from the internal organs, allowing the operation to proceed. Laparoscopic instruments are placed through the ports to perform the procedure.
The key steps of a safe cholecystectomy are the visualisation of the cystic duct (the tube from the gallbladder connecting to the main bile duct) and the cystic artery (the artery supplying the gallbladder). Once these structures are dissected out, small clips are placed on both the cystic artery and cystic duct. These clips stay inside the body and do not cause any issues. The gallbladder is taken out from one of the incisions, and the instruments are removed. The carbon dioxide gas is allowed to escape before the incisions are sutured with dissolving sutures.
Pre-Operative Assessment
Initial Assessment
Initial assessment will include blood tests and imaging of your gallbladder (Generally, an ultrasound scan would suffice). Additional imaging with an MRCP (Magnetic Resonance CholangioPancreatography) may be required if there are concerns about gallstones in the bile duct. The results of these investigations will be discussed with you, and treatment options will be outlined.
Anaesthetic Assessment
Once a decision has been made to proceed with surgery, you will be requested to fill out an anaesthetic questionnaire. This will be reviewed by the anaesthetist who will be responsible for your care. You may be required to see the anaesthetist in person or sent for additional tests. Once you have completed the anaesthetic review, the date of surgery will be confirmed with you.
Risk of Surgery
There are risks with any surgery, and they can be divided into “General” or “Procedure-specific risks.” Laparoscopic cholecystectomy is safe and one of the most commonly performed general surgical procedures. The risk of a serious complication is ~0.1% (1 in 1000 patients).
General Risks
- Wound infection
- Incisional hernia at the wound site
- Bleeding around the wound
- Venous thromboembolism (VTE), e.g. deep vein thrombosis (DVT) or pulmonary embolism (PE)
Procedure-Specific Risks from Laparoscopic Cholecystectomy
There are some rare but specific complications related to laparoscopic cholecystectomy:
- Bile duct injury
This is when the bile duct (which drains bile from the liver into the duodenum) is injured during a cholecystectomy. This is a very rare occurrence (~0.1-0.2%, 1-2 in 1000 patients) and usually occurs when the gallbladder is severely inflamed (cholecystitis). If there is a bile duct injury, a laparotomy (open incision) would need to be performed. The type of operative repair would depend on the severity of the injury.
- Post-operative bleeding
This usually occurs from the liver surface where the gallbladder is located, or from blood vessels surrounding the gallbladder. The incidence is around 1 in 300 patients. The bleeding generally self-resolves without any intervention required. You may need a blood transfusion and rarely, a re-operation may be required.
- Injury to surrounding bowel structures
There is a 1 in 300 incidence of injury to the surrounding bowel structures. This can be from the introduction of the laparoscope or instruments into the abdomen or from the dissection of the bowel structures adherent to the gallbladder. If there is an injury to the surrounding bowel, a re-operation will be needed.
- Open surgery
In some cases, open surgery is needed to complete the operation, which occurs in around 1-2% of cases. This is generally due to severe inflammation of the gallbladder with dense adhesions to the surrounding structures, precluding safe laparoscopic surgery. This involves a larger incision in the abdomen and requires a longer hospital stay after the operation.
- Common bile duct stones
In some cases, a cholangiogram (X-ray study of the bile duct) may be performed during the procedure, and stones are detected in the bile duct (Cholecystolithiasis). Some of these can be removed during the same procedure, but occasionally, it is not possible to complete it laparoscopically (most commonly due to the size of the stones). In that situation, an endoscopic procedure (ERCP) will be required to remove the stones at a later date.
Contraindications to Laparoscopic Surgery
All patients undergo a thorough assessment before deciding whether to proceed with a cholecystectomy. This will include clinical examination, blood tests, and imaging. Dr Michael Chu will work alongside you at each step of the assessment and make sure you have a thorough understanding.
In rare cases, such as severe lung disease precluding laparoscopic surgery or significant previous abdominal surgeries, an open cholecystectomy may be recommended instead. This is performed with an incision in the right upper quadrant of the abdomen. A longer hospital stay is expected after an open cholecystectomy.
Cholecystostomy
Post-Operative Management
You will be admitted to the ward for the night of your surgery, and the nursing staff will routinely perform a number of checks, including overnight. Most patients stay one night in the hospital and are discharged the next day. However, if the operation is done early in the day and is straightforward, discharge might be possible on the same day.
During your hospital stay, Dr. Michael Chu will review you twice a day. The ward staff are very experienced in caring for patients following gallbladder surgery and will care for you.
Post-Discharge Management
When should I seek medical input?
How does my General Practitioner (GP) know about my surgery?
Dr Michael Chu will send a letter summarising your hospital stay and a copy of your operation note to keep your GP up-to-date with your status. It is advisable that you make an appointment with your GP a few days after your discharge so they can physically assess your clinical status.
Common side-effects of surgery & solutions
- Pain or discomfort
After an operation, a degree of discomfort is expected and usually improves over the first two weeks. In some patients, the discomfort may last for a few weeks. The prescribed analgesia aims to ensure that the discomfort is manageable so you can continue improving physically. However, if the pain worsens or you have any concerns about its duration, please contact your GP or Dr. Michael Chu.
- Bruising
There is usually bruising around the incision, which may appear within 24-48 hours after surgery. If you feel that the bruising worsens, becomes painful, or there is discharge of pus from the wound, please contact Dr. Michael Chu.
- Constipation
This is a common occurrence following any abdominal surgery. It is usually related to the opioids during general anaesthetic or those given post-operatively for analgesia. A few laxatives can be obtained over the counter at the pharmacy or by prescription. Similarly, natural dietary supplements such as kiwi fruit are also quite effective. Importantly, please drink plenty of fluid.
Frequently Asked Questions about Liver Surgery
What is the recovery period?
The recovery period is at least 3-4 days before returning to normal activity. For an open cholecystectomy, the recovery period may be 4-6 weeks.
How soon can I drive after laparoscopic cholecystectomy?
It is usually recommended that you do not drive for 48-72 hours after laparoscopic cholecystectomy. When you get home and feel ready to drive, sit in the car seat and ensure you are able to perform a full emergency stop/brake before you start driving. It is also advisable that you have the strength to control the car and respond quickly before you start driving.
Importantly, please check with your insurance policy and company to ensure that driving post-operatively does not invalidate your policy.
Will my diet need to change after a cholecystectomy?
There are no dietary restrictions or requirements after a cholecystectomy. Most patients are able to have a diet similar to before the procedure, but some patients find that they are unable to tolerate a rich/fatty meal and have bloating and/or diarrhoea following the meal. This usually resolves as the body “resets” but may last for several weeks (6-8 weeks).
For 1 in 100 patients, they may have persistent diarrhoea and may require medical treatment that sequest the bile salts (such as cholestyramine).
What do I need to do to prepare for surgery?
Once a proposed date for surgery has been set, you will need to follow these instructions:
- Specific instructions will be given on where and when to present for surgery
- Specific instructions will be given on when to stop drinking and eating. It is important that you follow these instructions as it will pose an anaesthetic risk, and we may have to cancel/delay your surgery.
- You do not need to shave before coming into hospital
- You will be advised on what normal medications to take on the day of surgery, but only take them with a small amount of water.
- If you are on any blood thinners that affect clotting, please inform Dr Michael Chu during your initial consultation, as they may need to be stopped well in advance of the day of surgery. If you are unsure about the medications, please ask Dr. Michael Chu and the anaesthetist.
What is the follow-up process for me?
After you are discharged from the hospital, a follow-up will be arranged. Dr. Michael Chu’s PA will contact you, and the follow-up is usually 1-2 weeks after leaving the hospital.
At the follow-up consultation, Dr. Michael Chu will go through with you:
- How you are recovering
- Operative findings
- Pathology report from the surgery (This may take up to 3 weeks from surgery)
If you have any questions or concerns during your post-operative period, please contact Dr. Michael Chu at +64 27 216 7288.
